Understanding Diabetes: The Basics
Type 1 Diabetes (T1D):
Type 1 diabetes is an autoimmune condition in which the body’s immune system attacks and destroys the insulin-producing beta cells in the pancreas. Without sufficient insulin, blood sugar (glucose) can’t enter cells effectively, causing high blood sugar levels. People with Type 1 diabetes must use insulin therapy to survive. Currently, no definitive cure can fully restore the body’s natural insulin production and regulation.
Type 2 Diabetes (T2D):
Type 2 diabetes, on the other hand, is largely characterized by insulin resistance—a situation where the body’s cells don’t respond well to insulin—and sometimes reduced insulin production over time. It’s influenced by genetic factors, lifestyle elements (such as diet, physical activity, and body weight), and environmental components. Unlike Type 1, Type 2 diabetes can sometimes be driven into remission through lifestyle changes, certain medications, or bariatric surgery. While “remission” is often considered a form of reversal, it isn’t technically the same as a “cure,” because the underlying tendency toward impaired glucose metabolism can return if a person regains weight or reverts to old habits.
Going In-Depth on Each Key Point
1. Type 1 Diabetes: Why There’s No Current Cure
The autoimmune nature of Type 1 diabetes means the body’s immune system actively destroys the beta cells that produce insulin. For a cure, scientists would need to:
- Stop the immune attack on beta cells.
- Restore the body’s ability to produce its insulin, either by regenerating beta cells or transplanting functional cells that the immune system won’t destroy.
Research and Advances:
- Islet Transplants: Some progress has been made in transplanting islet cells from donors into people with type 1 diabetes, showing that normal blood sugar levels can be achieved for months or even years. However, the need for immunosuppression and the limited availability of donor islets are hurdles.
- Beta Cell Regeneration and Stem Cell Therapy: Emerging research on stem cells aims to produce insulin-producing cells that are genetically shielded from immune attack. Clinical trials are ongoing, but these approaches remain experimental.
What This Means ? :
There is no confirmed cure for type 1 diabetes today. Patients rely on daily insulin therapy, glucose monitoring, and newer technologies like continuous glucose monitors (CGMs) and insulin pumps. Although these improvements enhance quality of life and control, they do not eliminate the underlying condition.
2. Type 2 Diabetes: Remission Versus Cure
People with Type 2 diabetes may achieve sustained normal blood sugar levels without medication if they lose a significant amount of weight, adopt a healthy diet, and remain physically active. This state, often called “diabetes remission,” can last years, but isn’t guaranteed to be permanent.
Key Research on Remission:
- Dietary Intervention and Remission: A landmark trial known as the DiRECT study found that intensive weight management in primary care settings led nearly half of participants with Type 2 diabetes to achieve remission at one year. Patients lost substantial weight via a structured meal-replacement diet and then reintroduced healthy foods gradually.
What This Means ? :
While not a cure in the strictest sense, remission offers a path to living without the day-to-day burden of diabetes medications. It requires ongoing effort and may not be permanent if previous lifestyle patterns return.
3. Lifestyle Modification: The Cornerstone of type 2 diabetes Management
Even short of remission, improved glycemic control significantly reduces the risk of complications like nerve damage, eye disease, kidney problems, and heart disease. Increasing physical activity, improving diet quality, and maintaining a healthy body weight are crucial first steps.
Supporting Evidence:
- The U.S. Centers for Disease Control and Prevention (CDC) cites that regular physical activity, a balanced diet rich in whole foods, and modest weight loss (5-10%) can substantially improve blood sugar control.
4. Technological and Medical Advances
While type 1 diabetes and type 2 diabetes continue to be areas of intense research, medical technology is improving quality of life and glucose management strategies:
- Continuous Glucose Monitors (CGMs) help track blood sugar levels in real-time.
- Automated Insulin Delivery Systems (Artificial Pancreas) use algorithms to adjust insulin levels based on CGM readings.
Such developments streamline management, although they don’t constitute a cure. (Thabit H & Hovorka R. Lancet Diabetes Endocrinol. 2016;4(12):1005-1015.)
Visualizing the Complexity: A Simple Diagram
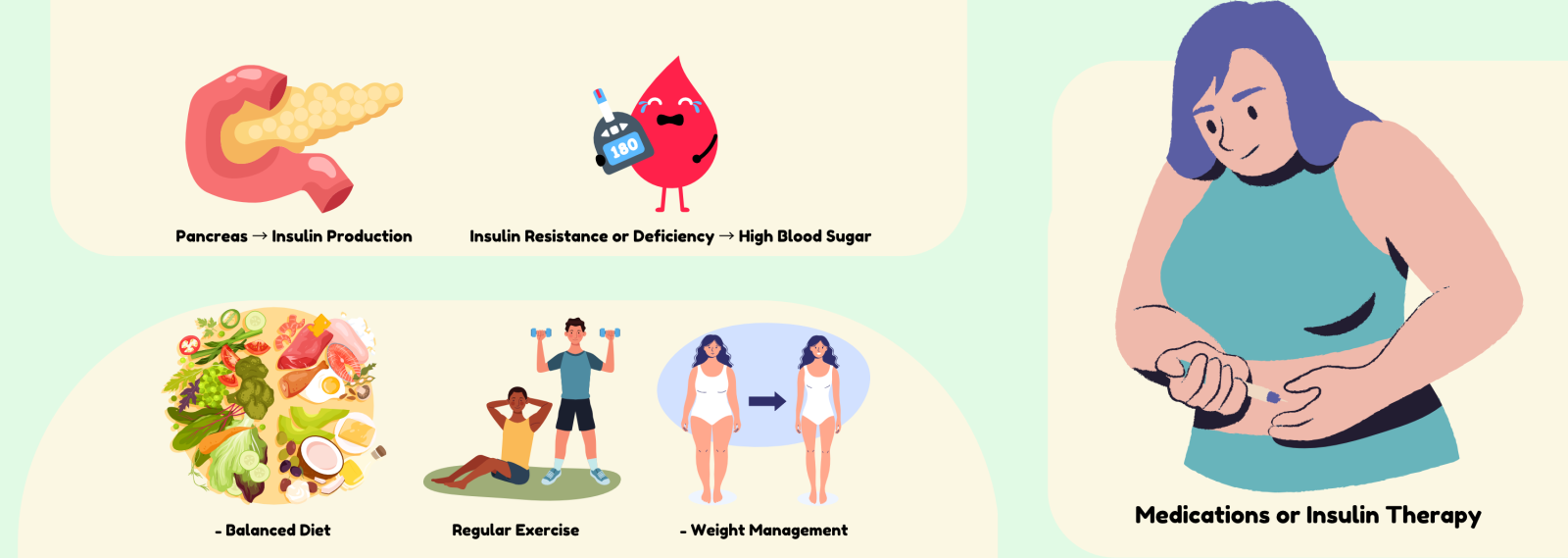
1. Biology & Insulin:
- Pancreas → Insulin Production
- Insulin Resistance or Deficiency → High Blood Sugar
2. Lifestyle Factors:
- Balanced Diet
- Regular Exercise
- Weight Management
3. Medical Interventions:
- Medications or Insulin Therapy
This triad helps people see how biology, lifestyle, and medical interventions intersect to manage diabetes.
Addressing Your Concerns and Emotions
It’s normal to feel scared, overwhelmed, or uncertain when facing a diagnosis of diabetes. You might fear complications or feel sadness about changing long-standing eating habits. Remember: You’re not alone. Millions of people live full, active lives while managing diabetes. Online forums, community support groups, and mental health professionals can all provide emotional support. Furthermore, doctors, nurse educators, and dietitians are trained to help you navigate these changes with compassion and practical guidance.
Taking Action: Concrete Steps You Can Begin Today
1. Know Your Numbers:
Measure your blood sugar regularly. Use a log or app to track your progress, and discuss the results with your healthcare team.
2. Incremental Diet Changes:
Swap refined carbohydrates (white bread, white rice) for whole grains, and increase your vegetable intake to improve blood sugar control.
3. Add More Movement:
Start with small steps—maybe a 10-minute walk after dinner—and gradually build up to 30 minutes of moderate activity most days. Physical activity improves insulin sensitivity and supports weight management.
4. Professional Support:
Certified Diabetes Care and Education Specialists are trained professionals who can help tailor strategies to your specific lifestyle and health status.
5. Continuous Learning:
Stay updated with reliable sources like the American Diabetes Association or the National Institute of Diabetes and Digestive and Kidney Diseases for the latest research and recommendations.
The Bottom Line
- Type 1 Diabetes: Not currently curable. Treatment focuses on insulin therapy and technological aids to maintain healthy blood sugar levels. Research into immunotherapy, stem cells, and islet transplantation is ongoing.
- Type 2 Diabetes: While not permanently “curable,” remission is possible through significant lifestyle changes, weight loss, and sometimes bariatric surgery. Keeping blood sugar levels in a healthy range can reduce or even eliminate the need for medication.
- Continuous Progress: Research steadily advances our understanding, leading to better management tools, more effective therapies, and, perhaps one day, a true cure.
In the meantime, the power to shape your health outcomes lies in informed choices, professional guidance, and a supportive network. Through knowledge and action, you can take charge of your diabetes journey.